For a century, the American Cancer Society has held up “early detection” of breast and other cancers as its mantra. Once, that made sense. But over the past few decades, the limitations of this approach have become increasingly apparent to researchers, physicians and other advocacy groups: Early detection may not save lives, and it can lead to unnecessary procedures. Yet the ACS has continued to insist that early detection was still the best way to find and treat the disease, and it demanded that Americans not skimp on regular breast exams and mammograms.
Finally, this past week, the organization announced a new policy. It conceded that women at average risk for breast cancer should begin annual screening at age 45 — not age 40, as previously prescribed — and that tests can become less frequent after age 54. Why did it take the nation’s most fervent anti-cancer group so long to grapple with new facts? The answer is a reminder that the best way to fight disease is with evidence — and that we should not pay for tests that are not effective, even if they are popular.
In 1913, when the ACS was founded as the American Society for the Control of Cancer, early detection was obviously the key. Cancer was seen as a fatal disease. People sat at home with enlarging masses, frightened to visit their doctors and hear the bad news. At New York- Presbyterian Hospital, admitted patients were noted to have waited for up to three years before seeking treatment.
Thus, the ACS inaugurated a campaign warning of cancer’s “danger signals.” It urged anyone with problems such as a breast mass, weight loss or irregular bleeding to see a doctor immediately. Such advice made sense. On average, people whose cancers were diagnosed at an earlier stage did better.
Early detection received a huge boost in the 1940s with the introduction of the Pap smear, in which doctors scraped a woman’s cervix, looking for abnormal cells that might become cancerous. The ACS vigorously promoted Pap testing with its Women’s Field Army, which enlisted women for a fee of $1 annually to “fight” cancer. Military metaphors, which persist today, sent an optimistic message that cancer could be “defeated” with enough effort. ACS officials who traveled the country promoting the Pap smear received standing ovations after their presentations. Indeed, Pap testing fulfilled its promise. Aggressive treatment of cervical lesions prevented cancer; mortality from cervical cancer dropped by 60 percent in the decades after 1950.
With this triumph in hand, the ACS turned to breast cancer. There was no Pap smear for the breast, but doctors could examine women’s breasts in the office, and women could examine them at home. Between 1950 and 1955, more than 5 million American women viewed an ACS film called “Breast Self-Examination.” Searching for cancers when they were small, the argument went, made much more sense than waiting until they were larger and more likely to have spread.
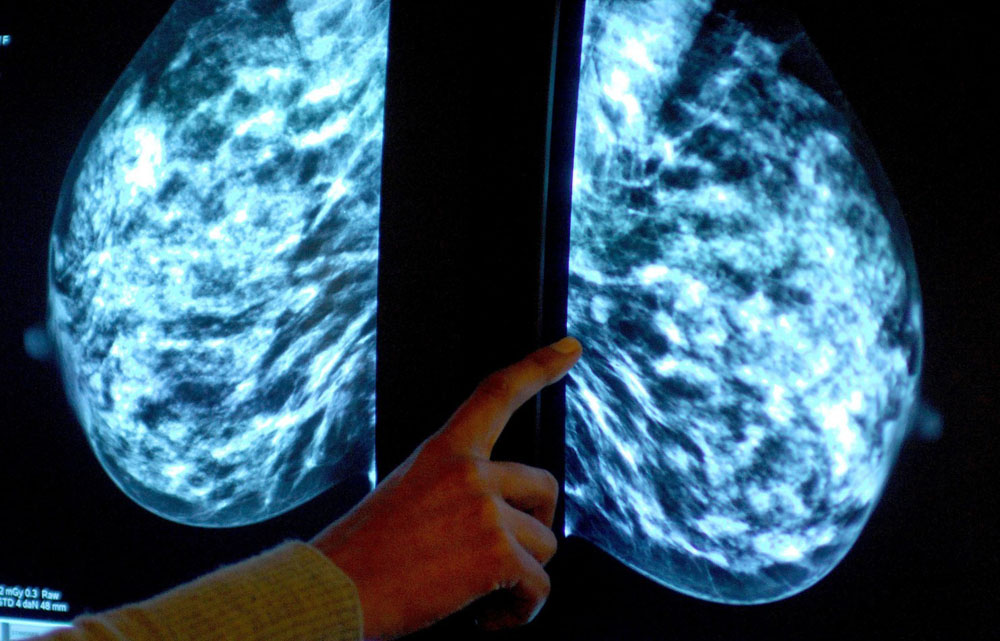
By the mid-1950s, radiologists were experimenting with mammograms, X-rays that could potentially identify even smaller breast cancers. Again, there was enormous enthusiasm. Women who declined screening, one physician wrote, were “playing Russian roulette with their lives.”
Hoping to achieve statistical proof, doctors who were optimistic about mammography decided to study it using randomized controlled trials in which some women were screened and a control group was not. There are now eight long-term trials of mammography based in the United States, Canada, Sweden and Scotland. And while there is debate about what these studies show, it’s clear that the technology is of little value for women under 50, whose relatively dense breasts make it hard to identify tumors on mammograms. One has to screen more than 2,000 women ages 40 to 50 annually for 10 years to save one life.
Meanwhile, all of this screening can cause harm. Annual doses of radiation may promote cancer. These women also will get unnecessary biopsies because some mammograms will show lesions that prove to be benign. One recent study found that this occurs in about 60 percent of women tested yearly in their 40s. For women over 50, mammography is a more effective tool, lowering mortality from breast cancer by roughly 20 percent. Breast examination, by doctors or women, has never been shown to prevent deaths from breast cancer.
Although disheartening and counterintuitive, this data makes sense. When the ACS began advocating for early detection, it believed that breast and other cancers stayed localized for years, spreading only late in their course. With this logic, an early and aggressive operation was crucial.
But as early as the 1950s, research indicated that some cancers actually spread early in their existence. Even if a cancer seemed localized to the breast at the time of detection and treatment, there were probably invisible metastases elsewhere in the body. The ability to eliminate these silent cancer cells with either hormone therapy or chemotherapy was more important than when the original cancer was identified and removed. And those treatments worked. Mortality from breast cancer, which was 31 per 100,000 women in 1975, declined to 21 per 100,000 women by 2010. Early detection — at least for older women — could help, but not nearly as much as the ACS publicity suggested.
Such a conclusion was difficult for the ACS to accept. The organization’s optimistic message that cancer was curable was predicated on its early-detection campaigns. ACS publicity pounded home the idea that all women over 40 needed annual breast cancer screenings. “If you don’t have your breasts examined,” one billboard announced, “you should have your head examined.” Any note of fatalism — that screening was pointless or of limited value — threatened not only the ACS’s image but also its ability to raise money for research and education. The value of early detection, it seemed at times, was as much cultural as scientific.
When John C. Bailar III, a biostatistician at the National Cancer Institute , began questioning the value of mammography in the 1970s, the ACS was resentful. At the time, it was conducting a demonstration project of mammography across the country in which more than 200,000 women would be screened. Bailar’s negative message, the ACS believed, was indirectly killing women. “As a clinician,” ACS Medical Director Arthur I. Holleb wrote in 1978, “I shudder to think of all the undiagnosed and unsuspected women with breast cancer who could be treated promptly and offered an excellent chance for cure.”
Even as other organizations, most notably the U.S. Preventive Services Task Force, progressively discouraged breast cancer screening, especially for younger women, the ACS held firm. Into the 1990s, it even recommended that women get a “baseline” mammogram in their late 30s, even though there was no evidence that such a test was effective.
But the ACS has finally changed its tune. Although the new guidelines leave room for more aggressive screening if women want it, those of average risk now need to have yearly mammograms only from age 45 to 54. After that, every two years is fine. And breast examinations by doctors are no longer recommended. For women at high risk, including those with a genetic mutation or a very strong family history, frequent screening is still advised.
Overturning the gospel has never been easy in medicine. Physicians like to practice medicine the way they learned it, and our reflexive tendency is to think that women cured of breast cancer were saved because they had a screening mammogram. So the ACS is to be applauded. Its new guidelines are based on the actual scientific value of early detection, not the organization’s needs and prior beliefs.
And more sensible guidelines could help save us money. Insurers generally pay for mammograms for younger women, despite knowing they lack value and can even cause harm. Given our historic trust in early detection, especially for breast cancer, this is not surprising. But in an era of cost containment, we need to prioritize payment for proven interventions — not simply those to which we are accustomed.
Originally published in the Outlook section of the Washington post, October 23, 2015.